Blocking an immune system molecule that accumulates after traumatic brain injury could significantly reduce the injury’s detrimental effects, according to a recent mouse study my neuroscience lab and I published in the journal Science.
The cerebral cortex, the part of the brain involved in thinking, memory and language, is often the primary site of head injury because it sits directly beneath the skull. However, we found that another region near the center of the brain that regulates sleep and attention, the thalamus, was even more damaged than the cortex months after the injury.
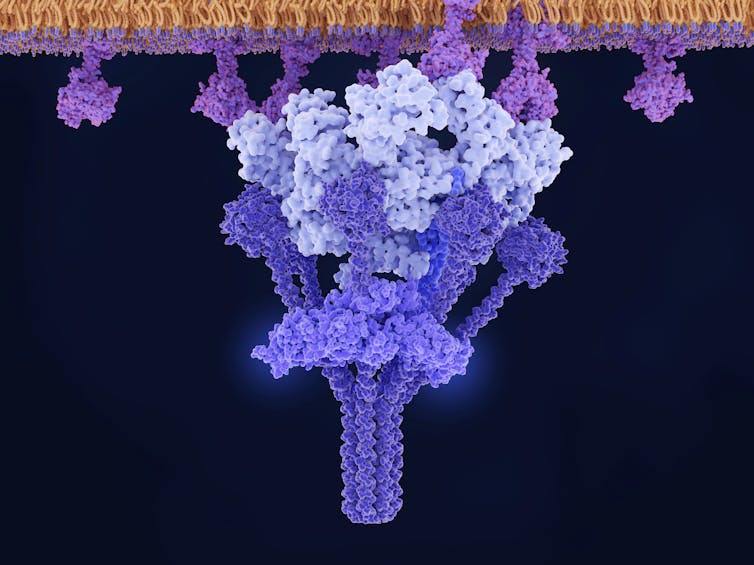
This may be due to increased levels of a molecule called C1q, which triggers a part of the immune system called the classical complement pathway. This pathway plays a key role in rapidly clearing pathogens and dead cells from the body and helps control the inflammatory immune response.
C1q plays both helpful and harmful roles in the brain. On the one hand, accumulation of C1q in the brain can trigger abnormal elimination of synapses – the structures that allow neurons to communicate with one another – and contribute to neurodegenerative disease. On the other hand, C1q is also involved in normal brain development and protects the central nervous system from infection.
In the case of traumatic brain injury, we found that C1q lingered in the thalamus at abnormally high levels for months after the initial injury and was associated with inflammation, dysfunctional brain circuits and neuronal death. This suggests that higher levels of C1q in the thalamus could contribute to several long-term effects of traumatic brain injury, such as sleep disruption and epilepsy.
C1q does provide some protection for the brain during traumatic injury, however. When we used genetically engineered mice that lack C1q at the time of trauma, the brain injury appeared much worse. This suggests that C1q is likely very important right when the injury happens in preventing cell death.
We collaborated with scientists at the biopharmaceutical company Annexon Biosciences to see if we could avoid C1q’s detrimental effects without losing its protective ones. We found that treating mice with an antibody that blocks C1q 24 hours after brain injury prevented detrimental effects like chronic inflammation and neuronal loss in the thalamus. Additionally, antibody treatment helped restore disrupted sleep spindles – these are normal brain rhythms during the early stages of sleep that are important for memory consolidation. It also prevented the development of epileptic spikes, or abnormal fluctuations in brain activity, which can disrupt cognition and behavior.
Why it matters
Traumatic brain injury can happen to anyone. It affects 69 million people worldwide per year and is a leading cause of disability in children and adults. Yet there are currently no therapies available to prevent the long-term disabilities that can result from brain trauma, such as epilepsy, sleep disruption and sensory processing difficulty.
We believe that targeting C1q after a brain injury could have protective benefits and help prevent some of the devastating consequences. Our study also answered some big questions in the field about where and how changes happen in the brain after trauma, and which ones actually cause deficits.
What still isn’t known
It remains unknown whether blocking C1q could also prevent epileptic seizures that develop after severe traumatic brain injury. Researchers are looking for biomarkers that would help identify people at high risk of developing epilepsy and working to understand the basic mechanisms leading from traumatic brain injury to epilepsy. There is no cure yet for post-traumatic epilepsy.
What’s next
My lab will continue working to expand our understanding of what happens in the brain after injury. Next, we want to focus on whether we can target C1q to prevent the convulsive seizures often reported among people with severe traumatic brain injuries.
C1q inhibitors are currently being tested in clinical trials for an autoimmune disorder known as Guillain-Barré syndrome. This could help accelerate treatment development for patients with traumatic brain injury.
This article is republished from The Conversation under a Creative Commons license. Read the original article.