Cancer treatment needs a reboot.
Despite the ambitious goals of the Biden administration’s “Cancer Moonshot,” which aims to cut cancer mortality by half over the next 25 years, progress is stalling in developing more effective therapies based on genetic information.
Simultaneously, the costs of cancer drugs are surging, often surpassing $20,000 per month. JAMA Oncology recently projected that between 2020 and 2050, the global cost of cancer will reach a staggering $25.2 trillion. This astronomical sum is in addition to the profound social and human cost of the disease.
An AI-based method is accurately pairing cancer patients with their most effective treatment.
Today, overall cure rates for advanced lung, breast, and colon cancer are typically less than 50%; most patients with these cancers will need a plan B after all the standard treatments have failed. We need a way to match approved or experimental cancer drugs to the patients whose tumors are likely to respond to them. Right now, though, deciding what treatments to try is largely guesswork, and success rates, when surgery fails to remove the entire mass, are depressingly low.
However, a glimmer of hope is appearing on the horizon, thanks to new approaches powered by AI. Although still in its early days, this method is already showing promising results — accurately pairing patients with their most effective treatment. And interestingly, the conceptual foundation of this approach comes not from oncology, but from astrophysics.
From stars to cells: Earlier this year, a collective of researchers and clinical investigators from Columbia, Mount Sinai Hospital, St. Jude, Emory, and other institutions, including one of us, published a groundbreaking clinical study in Nature Cancer.
The study used an innovative algorithm named VIPER (an acronym for “Virtual Inference of Protein-activity by Enriched Regulon analysis”) that demonstrated an unprecedented 100% accuracy rate in determining which patients with metastatic breast cancer would respond to a specific drug, called ricolinostat. Intriguingly, ricolinostat targets a protein encoded by a gene that does not mutate in cancer cells — challenging a common assumption that genetics is the only way to personalize treatment for individual patients.
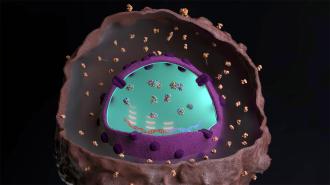
The VIPER algorithm — co-invented by one of us (Andrea Califano) and DarwinHealth Chief Scientific Officer, Mariano Alvarez — starts with what we can measure about a tumor but then delves beneath the surface to infer the hidden layer of master regulator proteins that drive the disease state of cancer cells. This feat was previously considered beyond our technological grasp. By analyzing gene expression profiles, it can decipher the unique pattern of master regulators in each tumor and the existing drugs that can deactivate them.
Selecting the right drug for a specific cancer patient has largely been a guessing game.
Interestingly, this approach shares parallels with astrophysics. Astrophysicists have long used inferential techniques to confirm the existence of celestial phenomena, such as black holes or exoplanets, which remain invisible to the naked eye. By applying these techniques at a microscopic level, we can start to unravel the hidden drivers of cancer cells.
These cancer-driving proteins are, like black holes, strange and elusive. Until recently, gauging their activity has been as challenging as trying to take a picture of celestial bodies that, like black holes, don’t emit or reflect light. Consequently, selecting the right drug for a specific cancer patient, particularly those who don’t respond to initial treatments, has largely been a guessing game, akin to trying to navigate a maze in the dark. It is a fantastically complicated maze, too: there are 250 FDA-approved cancer drugs and 200 different types of cancer, resulting in tens of thousands of possible drug-cancer combinations and literally billions more if you combine multiple drugs.
The findings reported in the Nature Cancer study could turn on the lights in this maze. The VIPER algorithm enabled scientists to infer the activity of a protein called HDAC6, which can act as an ignition switch for cancer, irrespective of any genetic markers or mutations. This highlights the potential to use treatments targeting proteins that aren’t necessarily linked to mutations, the most common basis for many expensive targeted cancer therapies.
Drugs prioritized by the algorithm predicted, with 91% accuracy, the ability to achieve disease control.
This translation of astrophysical techniques to cellular biology might sound straight from a science fiction novel, but it’s proving effective. VIPER, which also powers our biotech startup DarwinHealth’s drug discovery process — based on a model of cancer biology called “oncotecture” — acts like a cosmic detective. It takes measurable data, such as gene expression profiles, and uses it to make precise inferences about proteins most likely to have produced them, which are not directly measurable but can be decoded using a reverse-engineered biological model.
Further confirmation that the VIPER algorithm can predict a drug’s effectiveness was published on April 16 in the journal Cancer Discovery, in a study co-authored by one of us, as well as many other scientists from leading cancer research institutions around the world. Our experiment showed that drugs prioritized by the algorithm predicted, with 91% accuracy, the ability to achieve disease control in human tumors transplanted into mice. Notably, drugs favored by the algorithm significantly outperformed cancer drugs that were predicted not to work, which were used as controls.
People with rare, orphan cancers may especially benefit.
An even more recent study, just published in Cancer Cell, shows that VIPER can even be used to identify drugs targeting individual subpopulations of cells within a tumor. This is a critical feat because a tumor — just like cancer itself — is not all the same. A single tumor can harbor dozens of molecularly different subpopulations with different drug sensitivities, a phenomenon also known as cancer heterogeneity.
In a commentary published alongside the Nature Cancer study, a group of renowned outside cancer researchers described the innovative approach as “a roadmap for advancing cancer therapy.”
Indeed, such a roadmap is already leading to real world impacts. A clinical trial for children with metastatic Wilms and rhabdoid tumors is about to start enrolling patients. People with rare, orphan cancers like these, lacking targetable genetic mutations (including most children with cancer) may especially benefit here, working their way around the roadblocks affecting currently available approaches. The Cancer Discovery report also included a case study in a 14-year-old boy with a rare tumor that had progressed on all previous medications, but a drug predicted by the cancer algorithm was able to produce a durable two-year remission.
Trillions of dollars, countless lives: We believe the high cost and slow progress of cancer medicine today are, in part, rooted in the flawed assumption that genetics hold all the keys. While this is true for rare heritable diseases, the story is much more complicated for complex diseases, including most cancers, where proteins play a much more critical role.
Unfortunately, with few notable exceptions, even a precise understanding of a cancer’s genetic makeup — a routine test performed on people with cancer every day — can’t fully determine which drug or therapy will be most effective. For individuals with cancer, this often results in costly and physically debilitating cocktails of multi-drug interventions, many of which prove to be stabs in the dark that provide only marginal and transient benefits.
VIPER’s breakthrough lies in its ability to optimize the usage of existing drugs.
The new paradigm empowered by VIPER bridges the gap between patients and the drugs best suited to treat them, based on elusive protein targets known as “tumor checkpoints.” If this approach scales and is widely adopted, we believe this strategy could save trillions of dollars and countless lives by predicting more effective treatments for specific patient populations.
VIPER’s breakthrough lies in its ability to optimize the usage of existing drugs, freeing us from the costly process of new drug development, by connecting patients to FDA-approved drugs that can target the unique protein drivers of their tumors.
The improved drug-tumor alignments made possible by these AI-like approaches immediate cost savings. They promote the usage of approved, affordable, readily available drugs — but just importantly, they identify effective drugs early, when they’re most likely to work, reducing costs and toxicity from subsequent treatments when initial therapies fail.
While a comprehensive theory explaining cancer’s complexities remains elusive, we may be turning a corner with these protein-centric approaches. Cancer algorithms like VIPER could help us save lives, improve the quality of those lives, improve clinical trials’ accuracy, and reduce cancer’s projected multi-trillion-dollar cost over the next three decades. This new strategy, more akin to a “Cancer Starshot” than a “Cancer Moonshot,” offers a path forward in our ongoing battle with this devastating disease.
Dr. Gideon Bosker, MD, is CEO and co-founder of DarwinHealth.
Dr. Andrea Califano is the Clyde and Helen Wu Professor of Chemical and Systems Biology, Chair of the Department of Systems Biology at Columbia University Irving Medical Center, Director of JP Sulzberger Columbia Genome Center, and a member of the American Academy of Medicine. He is co-founder of DarwinHealth.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.