The man next to you coughs. You remember it is flu season. Your throat begins to feel a little itchy, and your body temperature starts to rise. It has only been seconds since the man coughed — far too soon for an infection to cause symptoms. Is it all in your head? Is the brain capable of causing these symptoms on its own?
Psychosomatic illness — a physical illness caused by mental factors, such as memories and emotions — is not a new idea. In fact, it might be one of the oldest medical models. In previous centuries, “mental factors” were described as an individual’s “spiritual factors.” Regardless of what you call them, they cause very real ailments: hypertension, chronic pain, impotence, and dermatitis, just to name a few.
It may come as no surprise that our brains store memories of past diseases. We are conscious of some of those memories: how miserable the symptoms were, the days spent in bed, the chicken soup. But most of the memories are stored in the subconscious, most notably, the memory of how the immune system responded to the disease. Studies over the last few decades have led scientists to believe that these “memories of immune responses” cause psychosomatic illnesses. Blocking these memories not only alleviates psychosomatic illnesses but “real” illnesses as well, according to a recent study published in Cell.
Memories of immune responses: a Pavlovian story
When Ivan Pavlov presented food to a dog, it began salivating. Pavlov began ringing a bell every time he presented food to the dog, and eventually, the dog was conditioned to salivate when it heard the bell, even in the absence of food. Essentially, the dog’s brain stored a memory of salivating after hearing a bell. So, when the dog heard a bell, its brain recalled that memory, determined that salivating is the appropriate response, and recreated that response.
In 1974, Robert Ader and Nicholas Cohen accidentally discovered the immune system can be conditioned in the same way. They were studying if mice could be conditioned to dislike a taste. They gave mice sweetened water, followed by an injection of a drug that causes nausea. After two months, the mice learned to avoid the sweet water after the initial taste. No surprise there. No one likes nausea, including mice. But then something unexpected happened: the mice that were forced to continue drinking the sweetened water started to die from infections at an alarming rate.
The drug they used to induce nausea also temporarily suppresses the immune system. The scientists had stopped giving the mice the drug, but even in the absence of the drug, the mice’s immune system was still being suppressed, thus they couldn’t fight simple infections. This meant that when mice tasted sweet water, the brain identified two typical responses: (1) avoid the water, and (2) suppress the immune system.
Ader and Cohen concluded that the brain stores memories of immune responses to stimuli; when it re-encounters those stimuli, the brain tries to replicate the previous immune response all by itself.
An immune response without a purpose
When a dog salivates, it causes a mess. If the saliva serves a purpose, the mess is worth it. But imagine a dog just salivating for no reason. That’s just slobber, and it’s not helpful to anyone. Immune responses are a lot like saliva: it always causes a mess (fever, inflammation, fatigue), but when there is a purpose (like protecting us from an infection), the benefit is worth the cost. An immune response without a purpose (like inflammation, arthritis, or allergies) is just an immune disorder and isn’t helpful to anyone.
Many psychosomatic illnesses are immune responses without a purpose. While you can avoid nuts to prevent an allergic reaction, how do you avoid memories to prevent psychosomatic illness? There has been little progress toward preventing and treating psychosomatic illnesses, largely because the region of the brain responsible for these memories has remained a mystery. Until now.
Remembering immune responses
A research group from the Technion’s Faculty of Medicine hypothesized that memories of immune responses are stored and retrieved by the insular cortex. The insular cortex is the region responsible for sensing the body’s physiological state (e.g., body temperature and nutrient levels) and interpreting them into bodily sensations (e.g., warmth and hunger). Previous research has shown that when the insular cortex is dysfunctional, immune response memories are not stored.
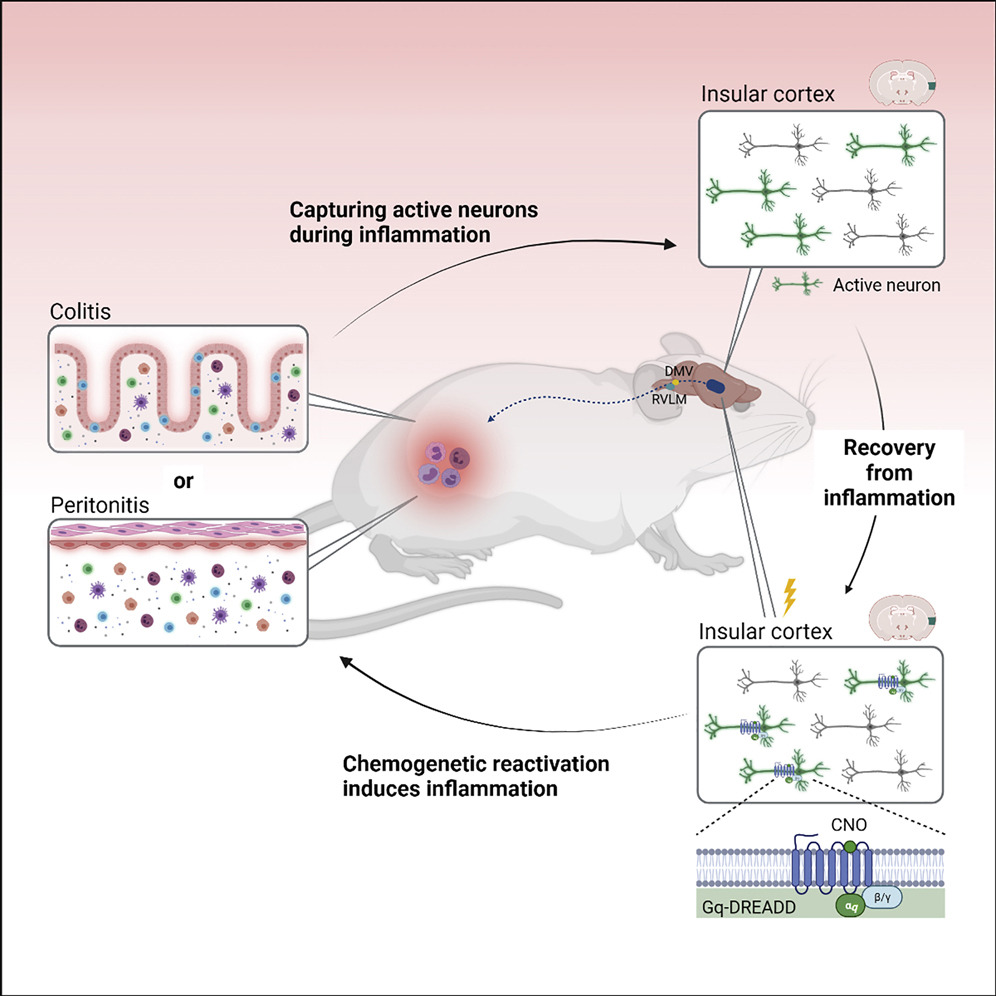
First, the researchers created the memory of an immune response. They induced gut inflammation in mice while monitoring brain activity and identified a group of neurons in the insular cortex with increased activity. The mice were given a month to recover from the disease state. Then, akin to a bell or sweetened water, the researchers used a sophisticated chemogenetic trick to trigger the memory that had been stored, selectively reactivating the same insular cortex neurons that were activated during the initial gut inflammation.
Without any outside stimulus (other than this activation of neurons), the inflammation returned, in the exact same location as it was originally. Simply “remembering” the inflammation caused the brain to reactivate it.
What if all diseases have a psychosomatic element?
Finally, the researchers were curious if the insular cortex played a role during the original inflammation experience or if it was just storing information to be retrieved later. In other words, was there a mental component involved in the non-psychosomatic disease from the very beginning?
Once again, they induced gut inflammation with external stimuli in mice that had no experience with the disease. However, this time, they inhibited insular cortex neuron activity. They found that the disease was significantly lessened, in terms of both clinical symptoms and immune response.
These findings suggest that even diseases that were previously thought of as non-psychosomatic might have a psychosomatic element, which worsens their effects. Identifying the role of the insular cortex in immune regulation opens the door to new ways of preventing and treating disease.
This article was reprinted with permission of Big Think, where it was originally published.